Continued from Part I…
So, I had survived after all. They’d performed the TURP while I was under anesthesia, and now, here I was. I could scarcely grasp the fact that the surgery was completed and I was actually in the recovery room. (These drugs: wow.) The nurses confirmed, at least a couple of times, in response to my continued expressions of disbelief, that yes, the surgery was over. I eventually developed an awareness that I felt pretty loopy but in no particular pain. Then someone called over from across the room, “Mr. Arnold, Katrina called.”
Ahhh…yes. Thank you very much! (Somebody called! Katrina called!)
And, then, I even took a phone call. In my first moments of consciousness, in typical TechnoMonk fashion I suppose, I had grabbed my bag and found my iPhone. Mere minutes later the phone started vibrating, so I answered it. The doctor’s office was on the line to reschedule the time of my first post-op appointment. Amazingly, I had the presence of mind to know what was going on; the new appointment time was there on my calendar later when I checked it.
 As time passed, the anesthesia, of course, began to wear off and I became more and more uncomfortable. I took the Vicodin that was offered, thankful that narcotics were available to ease my distress. Unfortunately, my body would not tolerate this painkiller. So, after the first 24 hours, I had no pain medication at all. My second day in the hospital was spent trying to reverse the effects (mostly intense stomach pain) of the Vicodin; it had actually caused more problems than it solved. I did experience some pain relief, during the first day and a half, with an occasional opium suppository. At one point I remember saying to the nurse, “I can’t believe I’m asking this, but could we do another one of those suppository things?” (I didn’t find out until later, though, that it was an opiate. Taking this approach to pain relief had its own consequences: I had a terrible rash on my butt for about the first 7 days after getting out of the hospital.)
As time passed, the anesthesia, of course, began to wear off and I became more and more uncomfortable. I took the Vicodin that was offered, thankful that narcotics were available to ease my distress. Unfortunately, my body would not tolerate this painkiller. So, after the first 24 hours, I had no pain medication at all. My second day in the hospital was spent trying to reverse the effects (mostly intense stomach pain) of the Vicodin; it had actually caused more problems than it solved. I did experience some pain relief, during the first day and a half, with an occasional opium suppository. At one point I remember saying to the nurse, “I can’t believe I’m asking this, but could we do another one of those suppository things?” (I didn’t find out until later, though, that it was an opiate. Taking this approach to pain relief had its own consequences: I had a terrible rash on my butt for about the first 7 days after getting out of the hospital.)
I awoke from the procedure with a catheter inside me. Now, that’s challenging enough, of course, but this happened to be a much-larger-than-your-average catheter, inserted right up into that place where there’s really no space.  It was connected to an IV kind of contraption that dripped fluid into me and constantly kept my insides flushed out, carrying away blood from my internal wound. For the next two days, it was my job to lie there patiently while I automatically peed out pink liquid into the bag tethered to the side of my bed. I ended up watching the bag with the source fluid very closely, making sure to call the nurse when it got too low. Everyone seemed entirely delighted by the color of the liquid that I passed – that it was merely pink, not too bloody red. So, of course, I was pleased that they were pleased.
It was connected to an IV kind of contraption that dripped fluid into me and constantly kept my insides flushed out, carrying away blood from my internal wound. For the next two days, it was my job to lie there patiently while I automatically peed out pink liquid into the bag tethered to the side of my bed. I ended up watching the bag with the source fluid very closely, making sure to call the nurse when it got too low. Everyone seemed entirely delighted by the color of the liquid that I passed – that it was merely pink, not too bloody red. So, of course, I was pleased that they were pleased.
The most significant source of stress for me while in the hospital was not actually the pain, though. My major issues had to do with privacy. And, no, not because of the nature of my surgery; I quickly became accustomed to having my gown lifted by anyone and everyone to check on my catheter and/or to insert a suppository up my rear. No problem. The big deal was trying to cope with my roommate(s). The room to which I was first assigned had another patient, in the next bed, who was so totally out of it that when my doctor visited the first evening, he asked that I be moved to a quieter space.
The room I moved to was even more problematic, however, and I spent almost 24 hours dealing with the antics of the new guy. He was in for knee-replacement surgery and obviously in much more pain than me. I don’t know how much of his behavior was drug-related, but the commotion surrounding him became a very big problem. He had a ridiculously loud, obnoxious, cell-phone ring tone, which seemed to go off constantly. And then, when someone wasn’t calling him, he was dialing out. 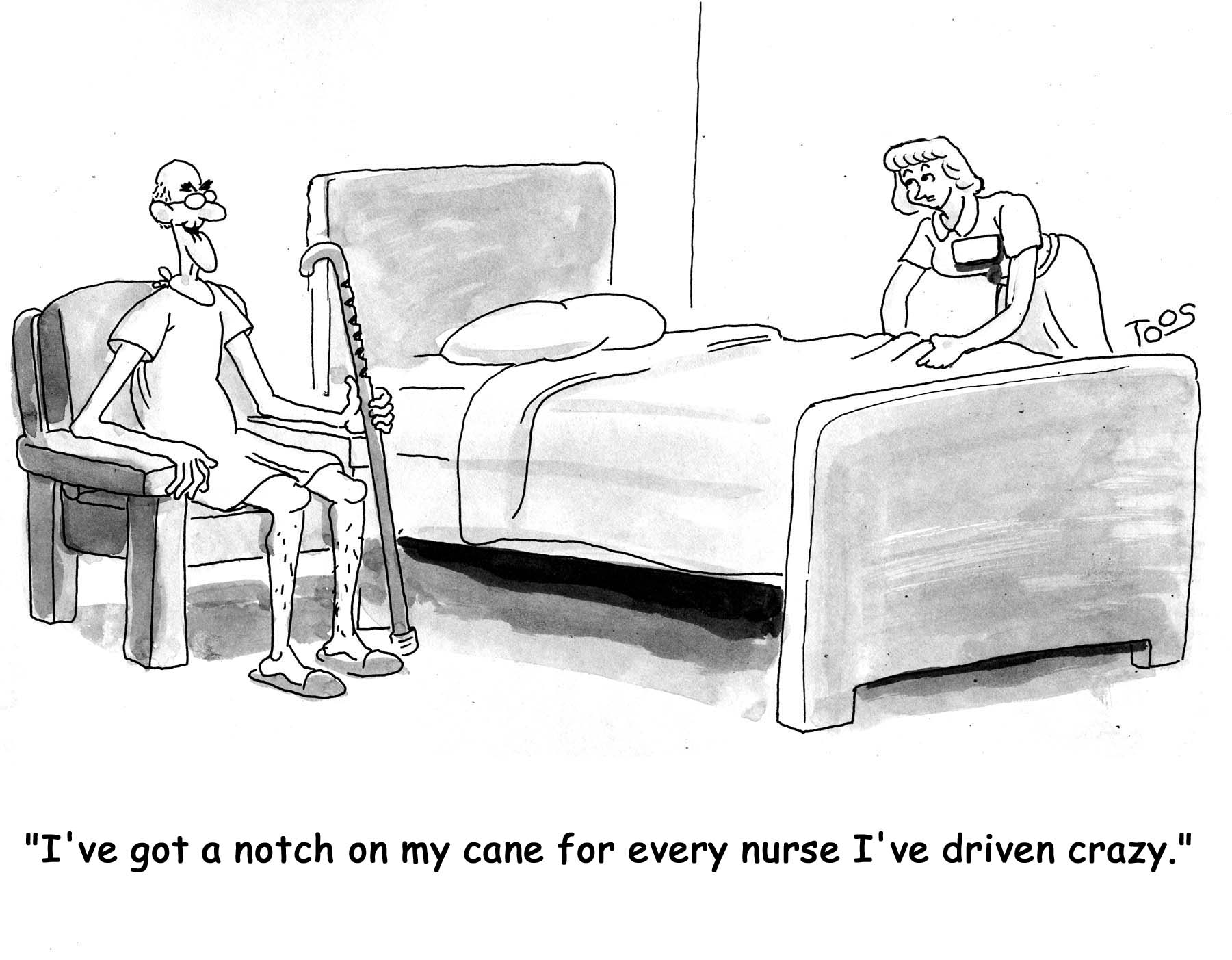 And he had one of those VERY LOUD TALKER cell phone voices that really intruded into my personal space. On top of all that, he had people needing to check up on him way more frequently than anyone was checking on me. If it wasn’t one thing, it was another.
And he had one of those VERY LOUD TALKER cell phone voices that really intruded into my personal space. On top of all that, he had people needing to check up on him way more frequently than anyone was checking on me. If it wasn’t one thing, it was another.
He even had an occupational therapist stop by to inform him that he was now going to need to put his pants on one leg at a time. (Did I really hear that correctly?!)
The most disruptive, and entirely outrageous, episode was when he guessed he could reach an item that was on a table close to his bed … but was clearly out of range. He kept reaching and stretching, stretching and reaching (when he should have been pressing the call button to ask for help), until he finally fell out of his bed. Yes, there he was, an old fart ten years my senior, needing to be totally immobilized because he was healing a new knee, and he literally took a nosedive off his bed. I said something like, “WTF, dude. What were you thinking?!” (… as he’s writhing in agony on the floor …) I pushed my button, and when they entered the room, the reason for the call was obvious. It took about 4 or 5 of them, as I recall, to lift him back onto his bed. Miraculously, he seemed to not have done any real damage to himself. But, oh my god, was this a noisy, upsetting, scene.
[The story continues here.]
[Technorati Claim: 3T2RHNHG8ZS9]