Entries in prostate surgery (7)
Roto-Rooter & Recovery: Part 5
 Sun, April 21, 2013 at 5:21PM
Sun, April 21, 2013 at 5:21PM Continued from Part 4…
Just after the three-month post-surgical mark, I had another follow-up appointment with my urologist. I had had some significant time to recover since the surgery, of course, and I wasn’t doing too badly. I was mostly-healed internally; thankfully, I had stopped peeing pink liquid. The continuing complaints I had were urgency and frequency with regard to my bladder behavior. I was also unhappy with the persistent tightness in my pelvic area that coincided with those symptoms and resulted in more trips to the restroom than I was really comfortable with. And the number of times I awoke during the night, to get up to urinate, continued to be problematic.
During this particular chat with the urologist, I made the observation that after years, yes decades, of frequent bathroom visits, I believed both my body and mind were still products of their long-term behavioral training. Despite the surgery, it appeared, my system was so accustomed to the bathroom ritual that it continued on, despite the radical intervention.
 The doc seemed to agree, and named other cases he had had that were similar to mine. He indicated that he been thinking about a strategy to address this condition: unfortunately, it involved yet another medication. He recommended a small dose of a low-risk, low-side-effect drug to control bladder behavior. (“It’s so mild they can give this to infants,” he said.) Although I wasn’t thrilled to take on yet another long-term medication (I had just recently disposed of my stash of Flomax, which I had been on for years), it seemed like a reasonable thing to try … especially when he indicated that we could view this as a temporary fix until my body could re-train itself. The drug involved is Oxybutynin, and I have been taking the 5-mg pill once a day since March 16, 2012 (just over thirteen months now).
The doc seemed to agree, and named other cases he had had that were similar to mine. He indicated that he been thinking about a strategy to address this condition: unfortunately, it involved yet another medication. He recommended a small dose of a low-risk, low-side-effect drug to control bladder behavior. (“It’s so mild they can give this to infants,” he said.) Although I wasn’t thrilled to take on yet another long-term medication (I had just recently disposed of my stash of Flomax, which I had been on for years), it seemed like a reasonable thing to try … especially when he indicated that we could view this as a temporary fix until my body could re-train itself. The drug involved is Oxybutynin, and I have been taking the 5-mg pill once a day since March 16, 2012 (just over thirteen months now).
For me, Oxybutynin has been only a partial solution. I had a short-term adjustment period getting used to the side effects (mostly dry mouth), but my body gradually came around to accepting the drug. And, over time, the tightness in my pelvic area became less pronounced and my bladder better behaved. However, given that I’m still taking it, this has obviously become a longer-term “temporary” fix than I’d anticipated.
A few months after I’d started on the Oxybutynin I was still having problems with frequency, so I was referred to a physical therapist specializing in bladder issues. (Yes, really, there are such therapists!) The whole physical-therapy experience will be the topic of my next entry.
 TechnoMonk
TechnoMonk
OK, I lied. I said I was going to continue on with my description of the prostate-surgery recovery, but, as you can see, I never did follow up. So, just let me try to tie up loose ends very briefly. I did see a physical therapist for a while and she was very helpful. The remedy, which turned out to be quite effective (in addition to the Oxybutynin medication), is a routine called “Kegel exercises” – or “pelvic floor exercises.” As I write this here, in March of 2015, I still do this every day, and control of my bladder remains manageable. For a description of this technique, click here.
Roto-Rooter & Recovery: Part 4
 Sun, March 4, 2012 at 3:46PM
Sun, March 4, 2012 at 3:46PM Continued from Part 3…
I bet you hope I’m getting close to wrapping up this series on my surgery. Perhaps I’ve paid so much public attention to it here because I don’t have an actual physical scar to show. All that pain and suffering, and no visible evidence. Drat!
 The last morning in the hospital looked to be pretty eventful. The surgeon was scheduled to remove the catheter, after which I would be allowed to go home. For the final procedure, he went about hunting down the numbing gel that was going to be needed; he’d specifically instructed the nurse to transport it to my new room the previous night. I directed him to the location where I believed it to be, and though it wasn’t exactly the substance he had ordered, he decided to use it anyway. (That made me a little nervous.) He briefly explained the extraction procedure to me and then, very quickly, it was over. I believe I let out a loud groan or gasp as it occurred, but the most intense part of the pain was fleeting. The cancer patient in the next bed, on the other side of the curtain, could hear the whole thing and offered up the opinion, “well, that sounded pretty ugly!”
The last morning in the hospital looked to be pretty eventful. The surgeon was scheduled to remove the catheter, after which I would be allowed to go home. For the final procedure, he went about hunting down the numbing gel that was going to be needed; he’d specifically instructed the nurse to transport it to my new room the previous night. I directed him to the location where I believed it to be, and though it wasn’t exactly the substance he had ordered, he decided to use it anyway. (That made me a little nervous.) He briefly explained the extraction procedure to me and then, very quickly, it was over. I believe I let out a loud groan or gasp as it occurred, but the most intense part of the pain was fleeting. The cancer patient in the next bed, on the other side of the curtain, could hear the whole thing and offered up the opinion, “well, that sounded pretty ugly!”
Post-catheter, I needed to hang around the hospital until I could successfully pee on my own. That happened quite soon, with a good, red, blood-drenched stream, which was accompanied by a lot of internal burning. As I would soon learn, this uncomfortable sensation would last awhile.
After the first bathroom visit was successful, I asked the nurse if I could call for my ride home. She said yes, so I made the call. I still needed to wait for final word from the doc, but it wasn’t long until he wandered by again, and said I was good to go (or, you know, something to that effect).
A friend picked me up and got me home. I remember almost falling down on the stairs leading to my apartment door, but being caught before I did damage to myself. I thought I was in pretty good shape that morning, but a few days later I realized I could barely remember the trip. I guess I was still under the influence.
In the weeks after the surgery, the recovery proceeded quite slowly. For the first ten days, I drank lots and lots of fluids to keep myself flushed out, which meant many trips to the bathroom. In terms of prostate symptoms, it seemed little had changed. I had my first post-op appointment ten days after surgery, though, and I was advised I could cut back on the fluids … and that, yes, things would settle down. In the next few hours, with less liquid intake, I did, indeed, need to make fewer trips. That was a huge relief.
 However, in coping with the rest of the recovery, patience seemed (seems) to be the key. I was very fortunate I had been able to time the surgery for early December. I missed three weeks of work and then a week when campus was closed entirely (for the holidays). During those four weeks, my energy was very low. It burned every time I peed. And I continued to bleed … for a long time. At the ten-day mark, I had reported the bleeding had ceased; that was definitely not the case. I bled for weeks and weeks. Sometimes a little bit, sometimes a lot; and just when I thought I’d bled for the last time, I’d bleed again.
However, in coping with the rest of the recovery, patience seemed (seems) to be the key. I was very fortunate I had been able to time the surgery for early December. I missed three weeks of work and then a week when campus was closed entirely (for the holidays). During those four weeks, my energy was very low. It burned every time I peed. And I continued to bleed … for a long time. At the ten-day mark, I had reported the bleeding had ceased; that was definitely not the case. I bled for weeks and weeks. Sometimes a little bit, sometimes a lot; and just when I thought I’d bled for the last time, I’d bleed again.
Although I am now able to manage life without taking Flomax (after ten years, being able to eliminate a major drug from my daily routine is very welcome), and my symptoms are much improved, I wonder if there will be a time when I stop thinking about the next bathroom trip. It seems that after years of conditioning, this is a hard habit to break, even when my body has had major work.
[The story continues here.]
Roto-Rooter & Recovery: Part 3
 Mon, February 20, 2012 at 10:51AM
Mon, February 20, 2012 at 10:51AM Continued from Part 2…
 After I’d been in this second room for about 24 hours, and not long after the roommate-nosedive episode, I told the nurses I simply couldn’t take it any more. I mean: really! I hadn’t slept my first night in the hospital, and I certainly was not going to sleep my second if I had to remain in the same space with Mr. Fruitcake. They finally agreed to move me yet again, though I couldn’t help but wonder what would happen next.
After I’d been in this second room for about 24 hours, and not long after the roommate-nosedive episode, I told the nurses I simply couldn’t take it any more. I mean: really! I hadn’t slept my first night in the hospital, and I certainly was not going to sleep my second if I had to remain in the same space with Mr. Fruitcake. They finally agreed to move me yet again, though I couldn’t help but wonder what would happen next.
So, my bed was rolled down the hall to another room about dinnertime, and although there was an occupant on the other side of the curtain, I heard nothing.
Ah … silence.
But, then, right around the time our meals were delivered, the guy’s family arrived: which appeared to be a wife and two small kids. Ugh. Still, everything worked out OK this time. They stayed less than two hours, and the kids were very well-behaved. Plus, I think the couple tried to talk so they couldn’t be overheard. Certainly, I could barely make out anything they said.
After his family left, I finally said “hi” – even though we couldn’t see each other. He indicated that he had had surgery for breast cancer a few hours earlier. He also said he had been diagnosed only a couple days ago; still, here he was recovering from surgery this evening. When I asked him a couple questions, he seemed to know precious little about his condition, which surprised me … but, then again, he’d only just been diagnosed and apparently had, on-faith, taken some doctor’s word for what needed to be done and when. I told him that I had gone through a breast-cancer experience with a former female partner in 1999 and she was fine, and that a male colleague of mine had had breast cancer in the early 2000s and his case turned out positively as well. I think he liked that report. In addition to clueless, he did sound a little scared.
 During the time I was in the hospital, just a little over 48 hours total, I had a couple of great nurses and a string of them that seemed, well, uninformed and uninvolved. The nurse who attended to me the first day, right out surgery, was very nice and genuinely concerned with attending to both my physical and emotional needs. However, the nurses who came and went during both nighttime hours, seemed totally oblivious to why I was there, what had gone on with me since I’d arrived, and were, quite-remarkably, disturbingly, detached. I did the best I could, through the fog of anesthesia, drugs, pain and fear, to keep track of what they were putting into my body and why, and what schedule I was on for what. As it turned out, I did a much better job of that than they ever did, even in my diminished-capacity condition. I pushed the button and told them it was time for this or that, and, when they looked it up on their computer, sure enough … there it was. When I was struggling mightily with the reaction I had to the Vicodin, on the morning after the surgery, in response to my request to figure out what was going on with my stomach pain, the nurse on duty said, “I need to check on something quickly, but I’ll be right back.”
During the time I was in the hospital, just a little over 48 hours total, I had a couple of great nurses and a string of them that seemed, well, uninformed and uninvolved. The nurse who attended to me the first day, right out surgery, was very nice and genuinely concerned with attending to both my physical and emotional needs. However, the nurses who came and went during both nighttime hours, seemed totally oblivious to why I was there, what had gone on with me since I’d arrived, and were, quite-remarkably, disturbingly, detached. I did the best I could, through the fog of anesthesia, drugs, pain and fear, to keep track of what they were putting into my body and why, and what schedule I was on for what. As it turned out, I did a much better job of that than they ever did, even in my diminished-capacity condition. I pushed the button and told them it was time for this or that, and, when they looked it up on their computer, sure enough … there it was. When I was struggling mightily with the reaction I had to the Vicodin, on the morning after the surgery, in response to my request to figure out what was going on with my stomach pain, the nurse on duty said, “I need to check on something quickly, but I’ll be right back.”
However, she didn’t return. And, when she did wander by about an hour later, I reminded her that I WAS STILL IN PAIN and could we do something, PLEASE?!
The computer system in the hospital was totally ridiculous. Every time the nurses had to check on ANYthing, they had to wait for the computer to boot up (very slowly), then they had to navigate to my records, check on the status and, finally, scan the barcodes on both the medication they were administering and on my wrist bracelet. Of course, this even included the Maalox and Tums they gave me for my Vicodin-induced stomach pain. What a joke. I told them that when I was sent a survey about my care at the hospital, I was going to advocate for a new computer system. (Which I subsequently did.)
In case you haven’t guessed: I really didn’t like being in the hospital.
[The story continues here.]
Roto-Rooter & Recovery: Part 2
 Thu, February 9, 2012 at 6:40AM
Thu, February 9, 2012 at 6:40AM Continued from Part I…
So, I had survived after all. They’d performed the TURP while I was under anesthesia, and now, here I was. I could scarcely grasp the fact that the surgery was completed and I was actually in the recovery room. (These drugs: wow.) The nurses confirmed, at least a couple of times, in response to my continued expressions of disbelief, that yes, the surgery was over. I eventually developed an awareness that I felt pretty loopy but in no particular pain. Then someone called over from across the room, “Mr. Arnold, Katrina called.”
Ahhh…yes. Thank you very much! (Somebody called! Katrina called!)
And, then, I even took a phone call. In my first moments of consciousness, in typical TechnoMonk fashion I suppose, I had grabbed my bag and found my iPhone. Mere minutes later the phone started vibrating, so I answered it. The doctor’s office was on the line to reschedule the time of my first post-op appointment. Amazingly, I had the presence of mind to know what was going on; the new appointment time was there on my calendar later when I checked it.
 As time passed, the anesthesia, of course, began to wear off and I became more and more uncomfortable. I took the Vicodin that was offered, thankful that narcotics were available to ease my distress. Unfortunately, my body would not tolerate this painkiller. So, after the first 24 hours, I had no pain medication at all. My second day in the hospital was spent trying to reverse the effects (mostly intense stomach pain) of the Vicodin; it had actually caused more problems than it solved. I did experience some pain relief, during the first day and a half, with an occasional opium suppository. At one point I remember saying to the nurse, “I can’t believe I’m asking this, but could we do another one of those suppository things?” (I didn’t find out until later, though, that it was an opiate. Taking this approach to pain relief had its own consequences: I had a terrible rash on my butt for about the first 7 days after getting out of the hospital.)
As time passed, the anesthesia, of course, began to wear off and I became more and more uncomfortable. I took the Vicodin that was offered, thankful that narcotics were available to ease my distress. Unfortunately, my body would not tolerate this painkiller. So, after the first 24 hours, I had no pain medication at all. My second day in the hospital was spent trying to reverse the effects (mostly intense stomach pain) of the Vicodin; it had actually caused more problems than it solved. I did experience some pain relief, during the first day and a half, with an occasional opium suppository. At one point I remember saying to the nurse, “I can’t believe I’m asking this, but could we do another one of those suppository things?” (I didn’t find out until later, though, that it was an opiate. Taking this approach to pain relief had its own consequences: I had a terrible rash on my butt for about the first 7 days after getting out of the hospital.)
I awoke from the procedure with a catheter inside me. Now, that’s challenging enough, of course, but this happened to be a much-larger-than-your-average catheter, inserted right up into that place where there’s really no space.  It was connected to an IV kind of contraption that dripped fluid into me and constantly kept my insides flushed out, carrying away blood from my internal wound. For the next two days, it was my job to lie there patiently while I automatically peed out pink liquid into the bag tethered to the side of my bed. I ended up watching the bag with the source fluid very closely, making sure to call the nurse when it got too low. Everyone seemed entirely delighted by the color of the liquid that I passed – that it was merely pink, not too bloody red. So, of course, I was pleased that they were pleased.
It was connected to an IV kind of contraption that dripped fluid into me and constantly kept my insides flushed out, carrying away blood from my internal wound. For the next two days, it was my job to lie there patiently while I automatically peed out pink liquid into the bag tethered to the side of my bed. I ended up watching the bag with the source fluid very closely, making sure to call the nurse when it got too low. Everyone seemed entirely delighted by the color of the liquid that I passed – that it was merely pink, not too bloody red. So, of course, I was pleased that they were pleased.
The most significant source of stress for me while in the hospital was not actually the pain, though. My major issues had to do with privacy. And, no, not because of the nature of my surgery; I quickly became accustomed to having my gown lifted by anyone and everyone to check on my catheter and/or to insert a suppository up my rear. No problem. The big deal was trying to cope with my roommate(s). The room to which I was first assigned had another patient, in the next bed, who was so totally out of it that when my doctor visited the first evening, he asked that I be moved to a quieter space.
The room I moved to was even more problematic, however, and I spent almost 24 hours dealing with the antics of the new guy. He was in for knee-replacement surgery and obviously in much more pain than me. I don’t know how much of his behavior was drug-related, but the commotion surrounding him became a very big problem. He had a ridiculously loud, obnoxious, cell-phone ring tone, which seemed to go off constantly. And then, when someone wasn’t calling him, he was dialing out. 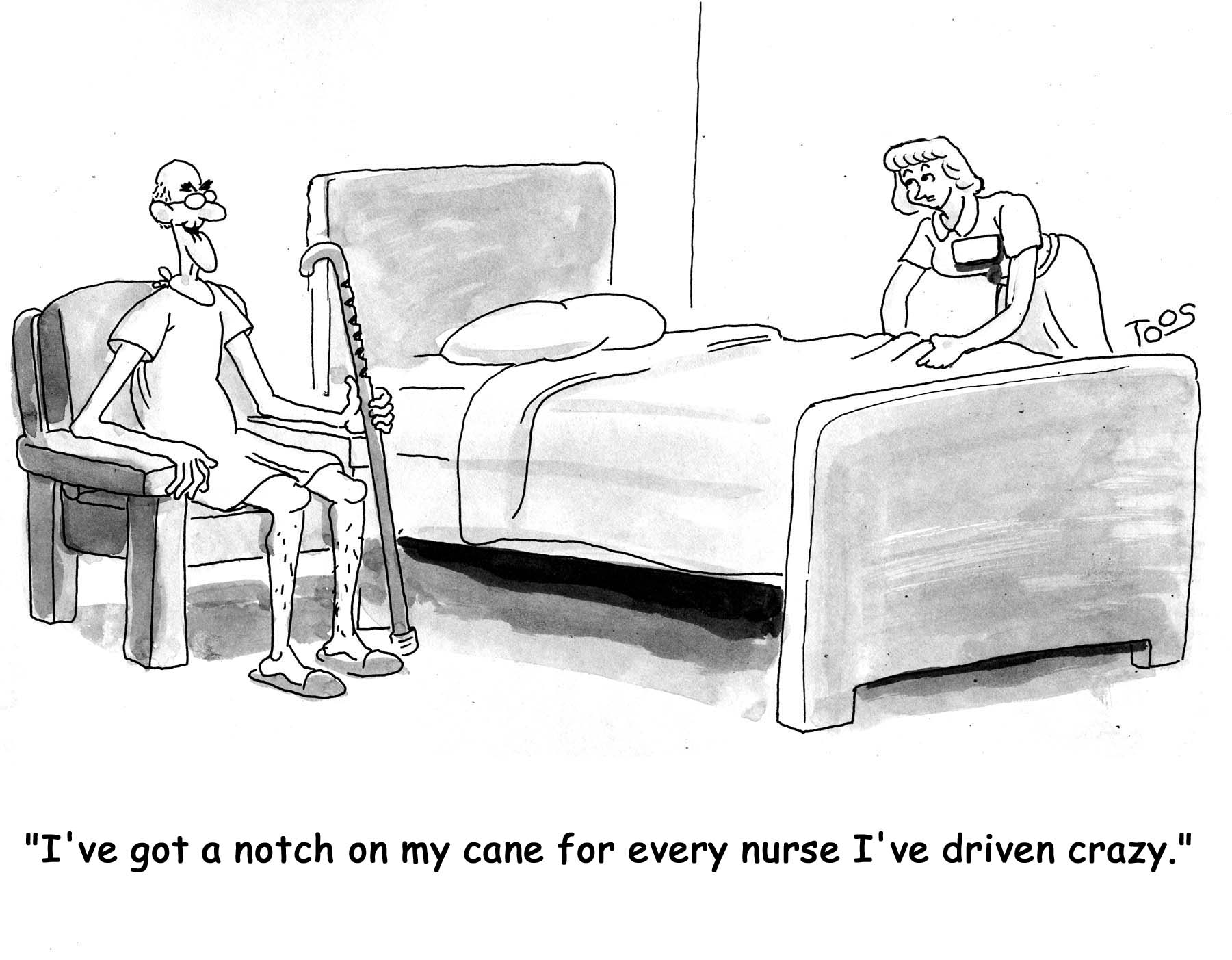 And he had one of those VERY LOUD TALKER cell phone voices that really intruded into my personal space. On top of all that, he had people needing to check up on him way more frequently than anyone was checking on me. If it wasn’t one thing, it was another.
And he had one of those VERY LOUD TALKER cell phone voices that really intruded into my personal space. On top of all that, he had people needing to check up on him way more frequently than anyone was checking on me. If it wasn’t one thing, it was another.
He even had an occupational therapist stop by to inform him that he was now going to need to put his pants on one leg at a time. (Did I really hear that correctly?!)
The most disruptive, and entirely outrageous, episode was when he guessed he could reach an item that was on a table close to his bed … but was clearly out of range. He kept reaching and stretching, stretching and reaching (when he should have been pressing the call button to ask for help), until he finally fell out of his bed. Yes, there he was, an old fart ten years my senior, needing to be totally immobilized because he was healing a new knee, and he literally took a nosedive off his bed. I said something like, “WTF, dude. What were you thinking?!” (… as he’s writhing in agony on the floor …) I pushed my button, and when they entered the room, the reason for the call was obvious. It took about 4 or 5 of them, as I recall, to lift him back onto his bed. Miraculously, he seemed to not have done any real damage to himself. But, oh my god, was this a noisy, upsetting, scene.
[The story continues here.]
[Technorati Claim: 3T2RHNHG8ZS9]
Roto-Rooter & Recovery: Part I
 Sun, January 29, 2012 at 3:01PM
Sun, January 29, 2012 at 3:01PM I had tried valiantly to avoid this operation for at least a decade. Of all the invasive procedures that can happen … I mean, wow. Not that I’d rather have brain surgery, of course, but still … here I was. The wait was over and the dreaded TURP was going to happen. This was the week I was going to show up at the hospital, point to my private parts, and say “have at it.”
 The morning before the surgery, the schedule called for me to go to the hospital and pre-register … which is a smart way to do things. This appointment did exactly what was intended: to save a lot of time during the day of the operation. I answered the receptionist’s and nurse’s questions (verified that I had not been taking blood-thinning drugs, for example), signed their forms, asked my own questions (can I bring my iPhone? my Kindle? my dietary supplements? – yes, yes, yes), and received my hospital wristband (along with the warning not to take it off or I’d have to do the check-in procedure all over again tomorrow). Then, I went to the lab for the final blood work, where I had to be stuck TWO times, by TWO techs, so they could do DUPLICATE tests. Oh, well, better safe than sorry?
The morning before the surgery, the schedule called for me to go to the hospital and pre-register … which is a smart way to do things. This appointment did exactly what was intended: to save a lot of time during the day of the operation. I answered the receptionist’s and nurse’s questions (verified that I had not been taking blood-thinning drugs, for example), signed their forms, asked my own questions (can I bring my iPhone? my Kindle? my dietary supplements? – yes, yes, yes), and received my hospital wristband (along with the warning not to take it off or I’d have to do the check-in procedure all over again tomorrow). Then, I went to the lab for the final blood work, where I had to be stuck TWO times, by TWO techs, so they could do DUPLICATE tests. Oh, well, better safe than sorry?
I did my best to keep breathing the rest of that day. The anesthesiologist called me in the evening for a short chat, and told me a little bit about the approach: we’d be using a spinal anesthetic, a technique that, when combined with the other drugs, would totally put me out, and also provide maximum benefit to the surgeon by relaxing my midsection for the work on my prostate. I wouldn’t remember a thing, he assured me.
That night I slept very fitfully and awoke early. According to instructions, I didn’t eat or drink anything. My ride was going to be here at 6:45 so I could be at the hospital by 7:00. Surgery was scheduled for 7:30.
The rest of the following two-day period (my time in the hospital) is somewhat of a blur. But I do remember parts …
The receptionist downstairs pointed me to the elevator. I went up to the waiting area and they almost immediately called my name. I was shown to a tiny curtained-off area where I was asked to disrobe and put all my belongings into a plastic bag. (Luckily, I had also brought along a gym bag to carry things in.) I put on the hospital garb and lay down. “Could I have another blanket, please?” They brought a nice, pre-warmed one. Ahhhh.
 Somebody came by and inserted an IV into my lower left arm. Poke. Ouch. The nurses were very nice, though business-like. The anesthesiologist came by and introduced himself. My urologist (the surgeon) stopped by to say hello and to let me know that we’d be underway shortly.
Somebody came by and inserted an IV into my lower left arm. Poke. Ouch. The nurses were very nice, though business-like. The anesthesiologist came by and introduced himself. My urologist (the surgeon) stopped by to say hello and to let me know that we’d be underway shortly.
Soon I was rolling down the hallway toward the operating room. We entered, I looked the place over, and said something like: “hmmmm… it doesn’t look like the Grey’s Anatomy rooms.” (I guess things are always different in real life, eh?) The put me on the table and …
… almost immediately I woke up in the recovery room: in the little curtained area where I’d left my stuff. What? It’s over?!? Really?
Well, of course it wasn’t over. The surgery was rather the easy part, even if it did involve inserting a tube up my penis and carving away part of my prostate. (They don’t call it a roto-rooter job for nothing!)
[The story continues here.]
